Corrales Ocular Innovation InstituteTM

Mission statement:
“To advance the art and science of ophthalmology through research and innovation”. We realize that graduating from medical school; specializing in ophthalmology; opening an office for treating and caring for patients was and is a very worthwhile and noble goal. Excellent patient care will always be our primary goal. However, those activities, alone, do not yield new devices and treatments to help patients. Only innovation from research advances medical treatment. This Institute does not perform non-innovative research such as reviews of the literature, reports of a series of operations, descriptions of diseases or cases, or quantification of former concepts. This Institute is, instead, dedicated to giving to patients and the medical profession new devices and treatments that will live beyond our doctors and their active years of practice.
Staff:
Gustavo Corrales, M.D. Founder, Medical Director
At the University of Pittsburg and New York Eye Institute he had advanced training in complex cataracts, corneal transplantation, and pterygium surgery. His research interests include developing pterygium surgery instruments, glaucoma, visual fields, and dry eye disease.
Diana Salazar Vega, M.D. Fellowship Trained Glaucoma Specialist
At the University of California at Los Angeles and at the University of Michigan she did outstanding research in visual field progression, outflow mechanism of glaucoma, and micro-glaucoma surgery.
John Karickhoff, M.D. Director of Research
Through extensive research, he is perhaps the only ophthalmologist to have produced a significant contribution or an innovation for each of the 14 anatomical parts of the eye.
- Kedrick Ng, Study Coordinator, Emerson Clinical Research Institute
- Lucia Munoz, Study Coordinator, Emerson Clinical Research Institute
- Christina Machuca, Certified Ophthalmic Technician
- Ihssane Moukad, Certified Ophthalmic Technician
- Jackie Serpas, Ophthalmic Technician
- Dario Peneda, Licensed Optician, Consultant
Private Practice Website:
Website of our private practice of ophthalmology is: www.NoVaVCS.com
Location and scope:

The Institute is located at:
410 S. Washington StreetFalls Church, VA 22046
Research Equipment
The Institute is in the office and uses the latest equipment of the medical practice of Dr. Corrales. This includes multiple slit lamps, cameras, lasers, surgical suite, OCT laser; computerized visual field machine; ultrasound machines; computerized keratometer, two corneal endothelial cameras, optical biometry, and others.


Ancillary research equipment of the Institute
Half of our research studies originate and are supported from Dr. Corrales’ private medical practice.
The other half of the research studies are done in association with the Emerson Clinical Research Institute. Dr. Corrales office contains the ophthalmic division of the Emerson Clinical Research Institute of Washington, D.C. which does human Clinical Trials on such diverse problems as Covid-19, urinary infections, and glaucoma. These studies are supervised by the United States Food and Drug Administration.
Our Seven Current Research Studies:
1) Corrales Floater Finder/Illustrator/Documenter
This Corrales floater documentation method is important because it tells the doctor which floaters are bothering the patient most. That may be different than the most prominent floaters seen by the doctor.
This Corrales method is especially valuable in locating an isolated, tiny floater in a young patient; and is especially revealing if the patient draws the floater much larger than it actually is.
Dr. Corrales has devised, tested, and perfected this method so that now each patient can see their floaters, differentiate solid (drawn green) from cloudy floaters (drawn yellow), locate them, draw them to scale, and signs the drawing. Their drawing is then photographed upside down and placed in their electronic record. When Dr. Corrales views the photograph, he sees the floater in its true position in the eye, not where the patient sees it. (All images are inverted inside the eye before reaching the retina.) The patient drawing is then used as an initial guide for Dr. Corrales’ examination. The patient’s floaters are then photographed; the drawing compared to the photograph; and finally Dr. Corrales makes his drawings for surgery.
Four steps of floater documentation:




2) Dry Eyes Study
 Some patients with Dry Eyes do not have an oily tear film layer to prevent evaporation of the tears. Seeing this oily layer is important in any study of dry eyes. A device developed here allows seeing and photographing this illusive multicolored oily layer.
Some patients with Dry Eyes do not have an oily tear film layer to prevent evaporation of the tears. Seeing this oily layer is important in any study of dry eyes. A device developed here allows seeing and photographing this illusive multicolored oily layer.
3) Device that improves visual field testing
Visual field testing is used to diagnose and follow patients with many diseases, especially glaucoma. Throughout the history of visual field testing, an opaque patch has been used to cover the eye not being tested. This results in complete darkness for that eye while there is the full brightness of the visual field machine shining in the tested eye. This sets up a rivalry between the two eyes, so that the vision of the tested eye blacks out intermittently (traditionally called Ganzfeld Blackout) during the test causing the patients to miss targets.
We devised a translucent difusser that blocks the vision of the non-tested eye but lets the full light of the machine to come into that non-tested eye. Ours is the first and only device that blocks the vision by diffusion, not occlusion. Thus, our device eliminates the rivalry and the missing the targets. Our device is called the “Corrales Visual Field Fatigue DiffuserTM.” All of our visual fields are done with this device. The device has been studied extensively in private practice and was found to make any visual field test less fatiguing; more accurate; and faster.
4) Device to aid in pterygium surgery

In the past the recurrence rate after surgical removal of a pterygium was as high as 70%. But with Dr. Corrale’s specialized training, using the latest techniques such as fibrin glue closure, conjunctival sliding flap, sometimes amnionic tissue and using the instrument he developed, his recurrence rate is less than 5%.
5) Study on treatment of dry eyes
Our double-blind study is to determine which eyedrops are the most effective in treating dry eyes.
6) Study on treatment of presbyopia

This study compares using eye drops to wearing glasses for reading.
7) Alternate glaucoma treatments
For patients who can’t handle eye drops for glaucoma or have a reaction to them, our study compares two alternative treatments: (a) laser treatment to the outflow channels of the eye, or (b) a medication pellet placed inside the eye.


8) Karickhoff Macular Acuity Tester - K-MAT
HAND-HELD DEVICE REVEALS MACULAR ACUITY
AND PREDICTS POST-OPERATIVE VISION
WHEN THE MACULA CAN NOT BE SEEN
By John Karickhoff, M.D.
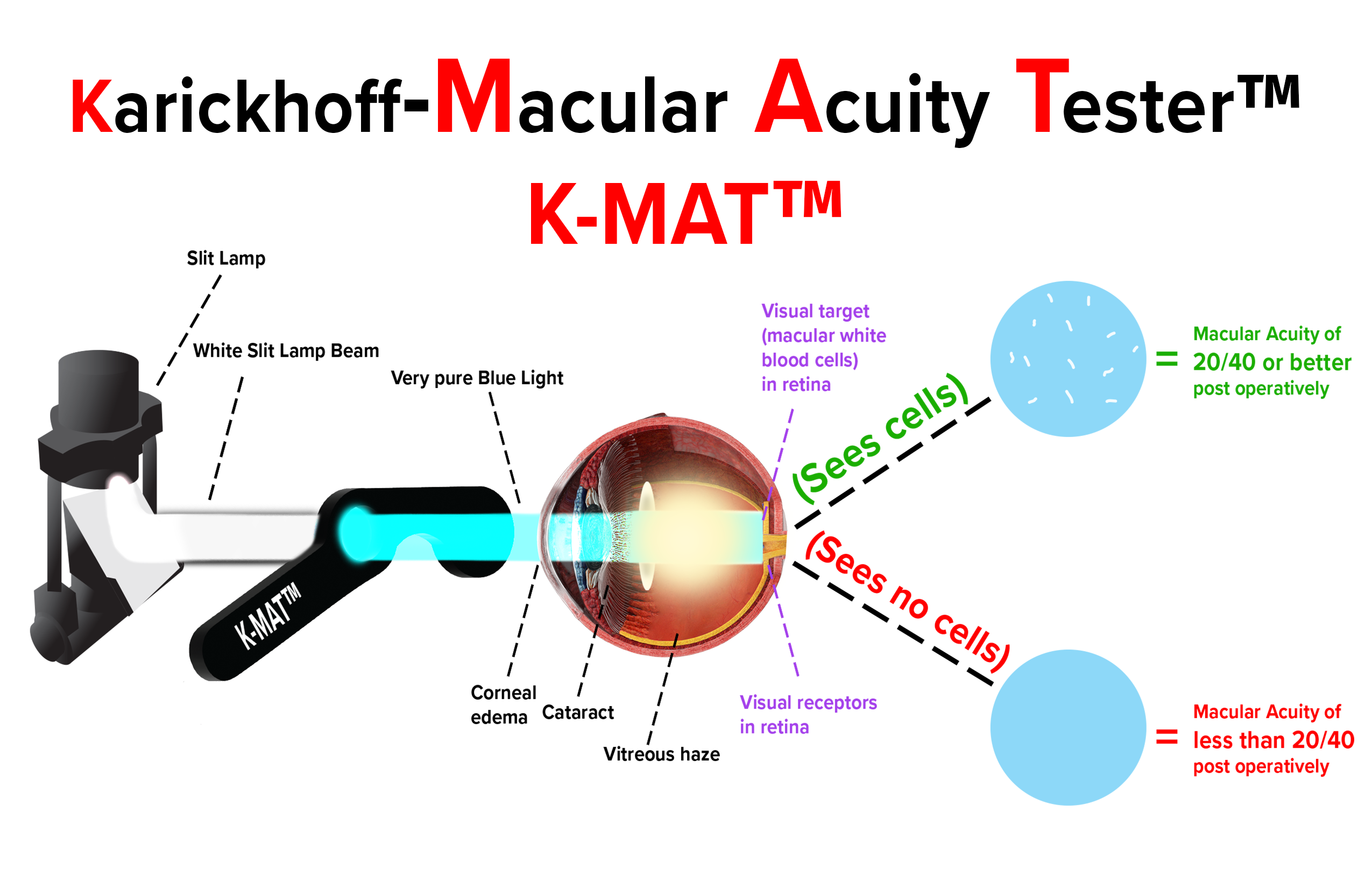
Doctors can easily examine the cornea, the lens, and the vitreous to learn if there is the clarity to allow good vision. However, learning the potential visual acuity of the macula when the cornea, lens, or vitreous is cloudy is presently impossible because the doctor (a) can’t see the macula adequately pre-operatively and (b) the cloudy cornea, lens, or vitreous blocks the macula from viewing the visual testing chart on the wall. To solve this impossibility, we are proposing using the blue-field entoptic test.
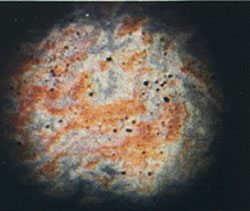
The blue-field entoptic phenomenon was first described in 1924 by Richard Scheerer. It consisted of using an electric light in a box as a projector to shine through a very pure blue light pass-filter into the eye of the patient. There the blue light was absorbed by the red blood cells in the micro-vessels of perifoveal area of the macula, but the light was not absorbed by the white blood cells. This created what appeared to the patient as about 50 tiny white lights each moving for about one second in its curved pattern and all lights pulsating when the patient’s heart beat.
We have studied this blue field entoptic phenomenon for 30 years and have learned or done six things with the test.
(1) We learned clinically that if the patient sees their retinal white blood cells in their perifoveal area, their macular acuity is 20/40 or better, which, by happy coincidence, is level of vision commonly used as the standard of surgical success.
(2) We learned that this test is independent of the presence of a cataract, vitreous or corneal haze as long as one gets some pure blue light to the retina.
(3) We learned that the test worked when the cornea, lens, or vitreous opacities were dense enough to prevent reading any conventional wall chart. This is possible because in this test, both the visual receptors and the visual target are adjacent in the retina, not one on the wall.
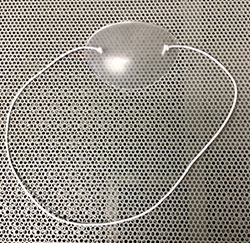
(4) We adapted the blue-field entoptic test from using the light in the box as the projector to using the slit lamp as the light projector. This was accomplished by simply placing the filter on a handle. This adaptation made the test less expensive, no table space was used, the patient did not have to be moved from the slit lamp to the box, and the test could be done in 10 seconds.
(5) We performed a 10-month clinical study to learn the accuracy of the test in predicting post-operative vision.
(6) We worked with a manufacturer and made this test commercially available.
The diagram shows how the test works: the bright, white light of the slit lamp shines through the proprietary filter which has the proper optical frequency bandpass, the proper band-width, diameter, and optical density so as to get adequate light to the retina but not to dazzle the patient. The blue light coming out of the filter into the patient’s eye, lights up their perifoveal white blood cells. This display is dramatic and unique for any viewer.