Corrales Ocular Innovation InstituteTM
“To advance the art and science of ophthalmology through research and innovation.”
We believe that graduating from medical school, specializing in ophthalmology, and providing excellent patient care are noble goals. However, true medical advancement comes from innovative research. Our Institute is dedicated to developing new devices and treatments, rather than conducting non-innovative studies, to benefit patients and the medical profession beyond our doctors’ careers.

Staff
Gustavo Corrales,MD, Founder, Medical Director
At the University of Pittsburg and New York Eye Institute he had advanced training in complex cataracts, corneal transplantation, and pterygium surgery. His research interests include developing pterygium surgery instruments, glaucoma, visual fields, and dry eye disease.
Diana Salazar, MD, Fellowship Trainer Glaucoma Specialist
At the university of California at Los Angeles and at the University of Michigan she did outstanding research in visual field progression, outflow mechanism of glaucoma and micro-glaucoma surgery.
John Karickhoff, M.D. Director of Research
Through extensive research, he is perhaps the only ophthalmologist to have produced a significant contribution or an innovation of each of the 14 anatomical parts of the eye.
Kedrick Ng, Study Coordinator
Lucia Munoz, Study Coordinator
Naty Flores, Certified Ophthalmic Technician
Jackie Serpas, Ophthalmic Technician
Research Equipment
The Institute operates in Dr. Corrales’ office, utilizing the latest medical equipment. This includes multiple slit lamps, cameras, lasers, a surgical suite, an OCT laser, a computerized visual field machine, ultrasound machines, a computerized keratometer, two corneal endothelial cameras, optical biometry, and more.

Half of our research studies are supported by Dr. Corrales’ private practice. The other half are conducted with the Emerson Clinical Research Institute, which has an ophthalmic division in Dr. Corrales’ office. This division performs FDA-supervised clinical trials on issues such as COVID-19, urinary infections, and glaucoma.
Innovation Studies
Corrales Floater Finder/Illustrator/Documenter
The Corrales floater documentation method identifies which floaters bother the patient most, which may differ from those seen by the doctor.
This method is especially useful for locating small floaters in young patients and is revealing when patients draw floaters larger than they are.
Dr. Corrales has perfected this method, allowing patients to see and differentiate floaters, draw them to scale, and sign the drawing. The drawing is then photographed upside down and added to their electronic record. Dr. Corrales views the photograph to see the floater in its true position in the eye. The patient’s drawing guides Dr. Corrales’ examination, and comparisons are made between the drawing and actual photographs before surgery.
Four steps documentation:




Translucent Occluder Significantly Improves Visual Field Testing
Early Design of Translucent Diffuser
Visual field testing is crucial for diagnosing and monitoring diseases, especially glaucoma. Traditionally, an opaque patch covers the non-tested eye, creating darkness and causing visual rivalry, leading to intermittent blackouts and missed targets.
We developed a translucent diffuser that blocks vision but allows light into the non-tested eye, eliminating rivalry and missed targets. This unique device, the “Corrales Visual Field Fatigue Diffuser™,” improves accuracy, reduces fatigue, and speeds up the test. All our visual field tests use this device, proven effective through extensive private practice studies.

Final Magnetic Translucent Occluder
During our research with the translucent eye patch above, we experimented and did a formal visual field study on 60 eyes to see if the patch had to be attached to the patient’s head over their eye as had been done since the inception of visual field testing. We found that by using our translucent diffuser and placing it on the visual field machine rather than on the patient’s head, it improved visual fields and visual field testing in 18 ways without the need of an eye patch! Our device was so successful that Haag-Streit of Switzerland, the world’s largest manufacturer of professional ophthalmic equipment, incorporated our Corrales/Karickhoff Diffuser with their Octopus 600 visual field machines, the most popular machine in the world.
You can obtain the occluder directly from Haag-Streit
Dry Eyes Study
Some patients with Dry Eyes do not have an oily tear film layer to prevent evaporation of the tears. Seeing this oily layer is important in any study of dry eyes. A device developed here allows seeing and photographing this allusive multicolored oily layer.
Device to Aid in Pterygium Surgery
In the past, the recurrence rate after pterygium surgery was as high as 70%. With Dr. Corrales’ specialized training and techniques, including fibrin glue closure, conjunctival sliding flap, amnionic tissue, and his developed instrument, the recurrence rate is now less than 5%.

Study in the treatment of dry eyes

Study on treatment of presbyopia
This study compares the effectiveness of using eye drops versus wearing glasses for reading.

Alternate Glaucoma Treatments

Laser treatment

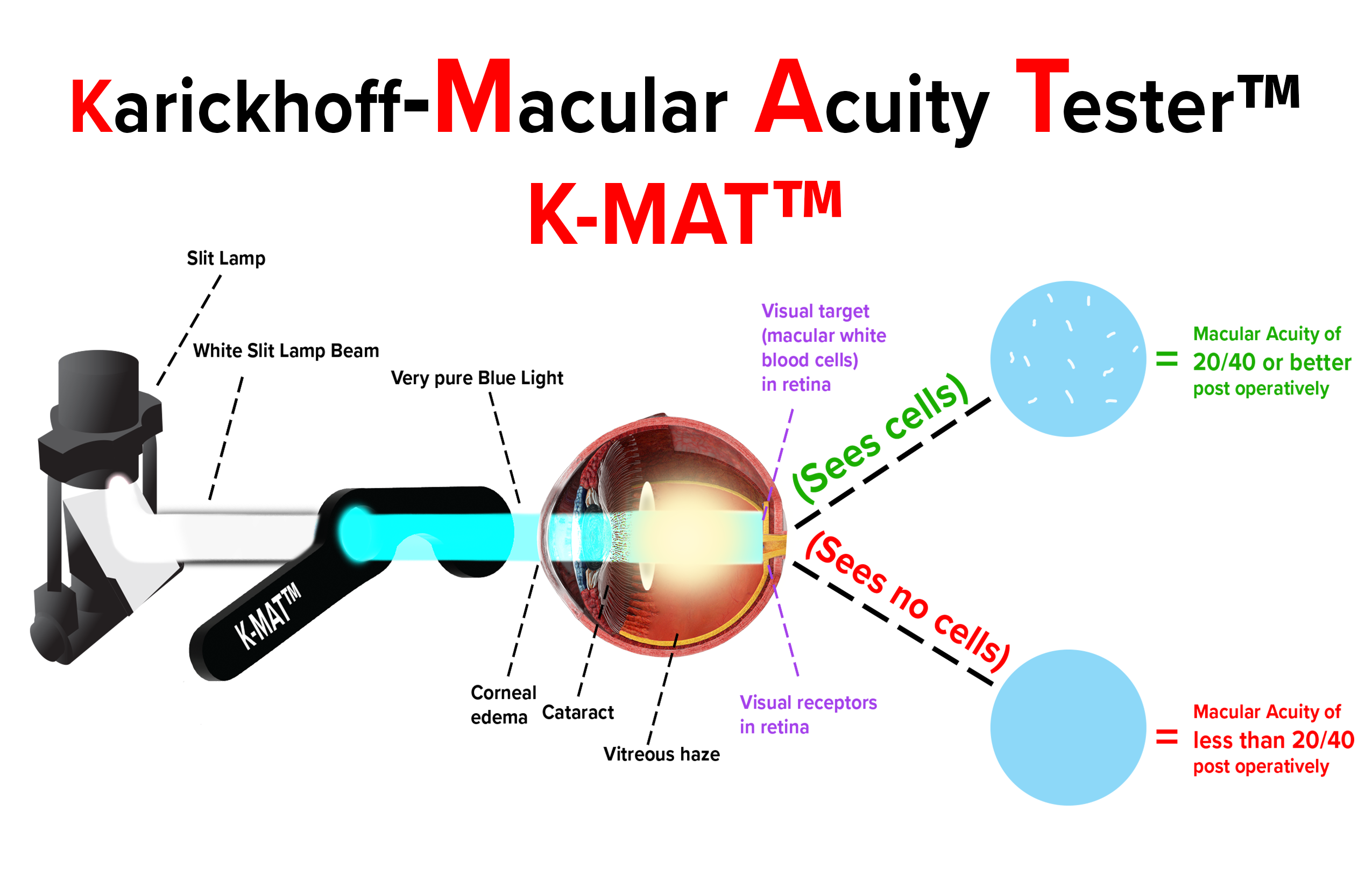
Karickhoff Macular Acuity Tester – K-MAT
Private Practice Website:
Website of our private practice of ophthalmology is: www.NoVaVCS.com
Location & Scope:
410 S. Washington Street
Falls Church, VA 22046
