Karickhoff Macular Acuity Tester – K – Mat
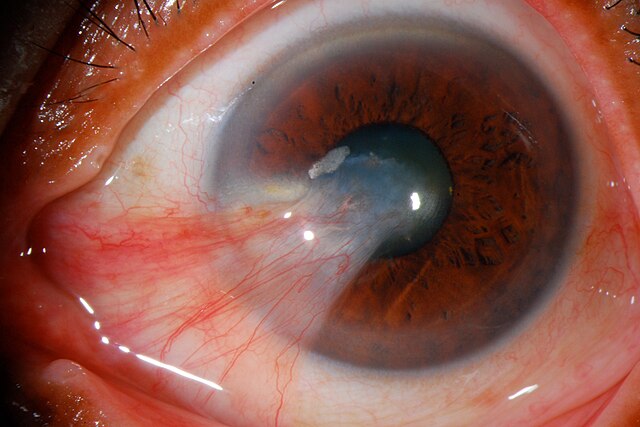
Safety and Efficacy of CBT-001 Ophthalmic Solution in Patients With Pterygium (Pterygium)
Pterygium is a noncancerous growth that may occur in one or both eyes. It usually causes:
• redness
• irritation
• eye discomfort
• blurry vision
This study evaluates the efficacy and safety of an eye drop to relieve the symptoms and possible decrease the size of the pterygium.
Official Title and Additional Information:
If you are interested in applying to this study please you can get in contact with one of our coordinators at 202-239-0777 ext: 102
